A recent case, Does it look like the sinus membrane is perforated?, prompted us to do a bit more research on the current thinking regarding sinus membrane perforation.
Sinus membrane perforation (SMP) is a common complication during sinus floor elevation procedures. As summarized below, various studies have explored the risk factors, treatment outcomes, and repair techniques for SMP.
-
Risk Factors and Outcomes: A study identified maxillary sinus contours and sinus membrane thickness as significant risk factors for SMP. The perforation rate was higher in narrow tapered sinus contours and when the membrane was thinner than 1 mm. Despite these perforations, no complications were observed upon recall when treated with collagen membrane coverage.
-
Repair Techniques: Different approaches have been used to repair SMP, including the use of resorbable collagen membranes, periosteal grafts, and innovative suturing techniques. These methods have been shown to effectively seal the sinus and support successful implant placement without increasing the risk of implant loss.
-
Alternative Materials: Platelet-rich fibrin (PRF) has been considered an alternative material for repairing sinus perforations due to its autogenous nature and ease of manipulation. It has been associated with increased bone formation and successful implant survival rates.
-
Success Rates of Implants in Sinus Membrane Perforation: The success rate of grafts and implants remains high even in cases of SMP. Studies have reported success rates of over 97% for both grafts and implants, indicating that SMP does not significantly compromise the outcomes when appropriately managed.
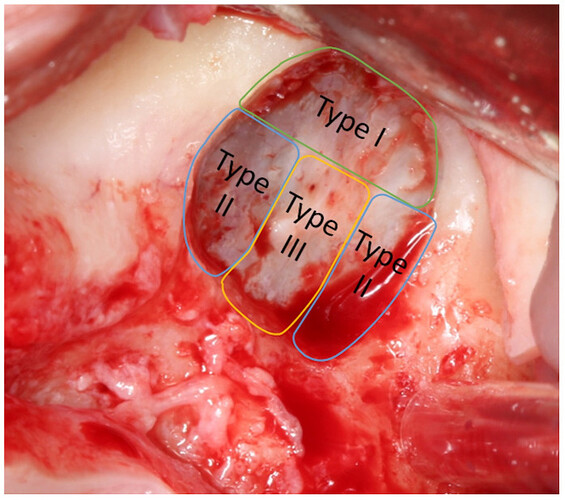
So considering the research, while SMP is a frequent complication, various effective repair techniques and materials are available to ensure successful treatment outcomes. The success of any treatment plan, of course, depends on the classification of the perforation, as shown in the image below.
Classification of the Perforation is Critical for Determining the Proper Plan
Image Source: Schiavo-Di Flaviano V, Egido-Moreno S, González-Navarro B, Velasco-Ortega E, López-López J, Monsalve-Guil L. I[nfluence of Schneiderian Membrane Perforation on Implant Survival Rate: Systematic Review and Meta-Analysis] (Influence of Schneiderian Membrane Perforation on Implant Survival Rate: Systematic Review and Meta-Analysis - PMC). J Clin Med. 2024 Jun 27;13(13):3751. doi: 10.3390/jcm13133751. PMID: 38999315; PMCID: PMC11242322.
Diagram illustrates the classification of the perforations of the maxillary sinus membrane described by Fugazzotto and Vlassis in A simplified classification and repair system for sinus membrane perforations. Fugazzotto and Vlassis proposed a classification for perforations according to size and the difficulty of reparation. Class I perforations are those that occur in the upper part of the osteotomy; the separation of the membrane from the bone will eventually close due to membrane folding upon itself. Class II occurs close to the lateral or lower walls of the osteotomy and its treatment is more complex. Class III perforations are located right in the center of the osteotomy window and are frequently preexisting, either due to a previous traumatic dental extraction or an oroantral fistula, although they can occur during the preparation of the membrane as well; their clinical management is similar to those of class II
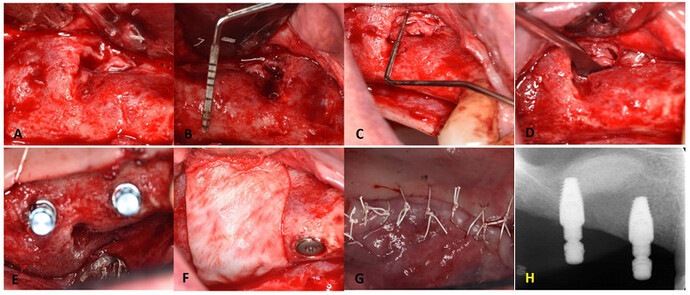
Quick Case: Repair of Sinus Membrane Perforation with Collagen Membranes and PRF
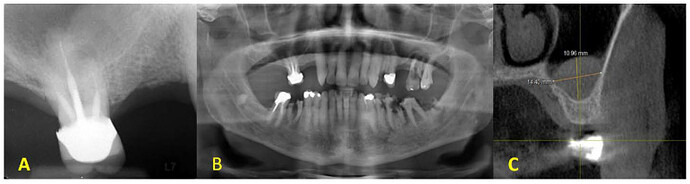
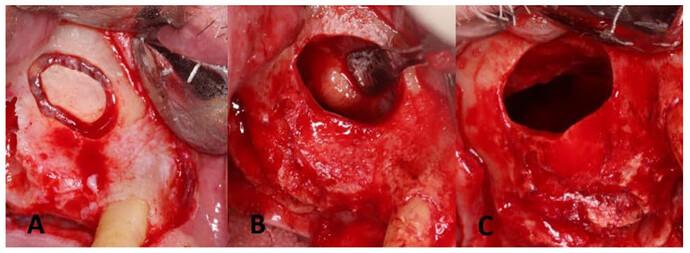
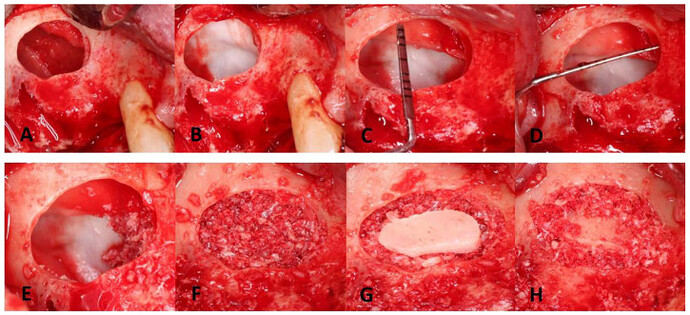
Image Source: Koleilat A, Mansour A, Alkassimi FM, Aguirre A, Almaghrabi B. A Combination of Platelet-Rich Fibrin and Collagen Membranes for Sinus Membrane Repair: A Case Report (Repair of Sinus Membrane Perforation). Dent J (Basel). 2023 Mar 17;11(3):84. doi: 10.3390/dj11030084. PMID: 36975581; PMCID: PMC10047151.
Preoperative radiographic evaluation: (A ) homogenous solitary radiopaque mass observed on the right sinus floor in intraoral periapical with a periapical lesion on the MB root of the right maxillary molar; (B ) a panoramic radiograph prior to initial therapy; (C ) CBCT cross-sectional view of mucocele/antral pseudocyst with a patent osteomeatal complex.
Lateral window preparation and the maxillary sinus cyst removal: (A ) lateral window preparation with Piezo surgery; the bony island was detached and saved in saline; (B ) sinus membrane after elevation and identification of the antral pseudocyst; (C ) sinus membrane perforation after specimen removal.
Membrane elevation with perforation repair and bone grafting: (A ) sinus membrane elevation; (B ) sinus repair with the first layer of CollaTape; (C ) apico-occlusal dimension = 10 mm; (D ) mesiodistal dimension = 10 mm with PRF membrane in place; (E ) placement of a BioGide membrane to properly seal the perforation site. Note the bone graft on the anterior medial portion; (F ) bone grafting of the surgical site well packed crestally; (G ) the bony wall was placed over the lateral window, and then the crestal portion then the sinus cavity was filled; (H ) bone graft around the bony island to stabilize the bony island.
Surgical re-exposure for implant placement: (A ) flap refection and exposure of previous sinus window; (B ,C ) adequate width and height for implant placement. Partial healing of the sinus window with evidence of fibrotic sinus membrane; (D ) mini-sinus lift through the residual antrostomy; (E ) implant placed in the prosthetic position; (F ) collagen membrane placed over the antrostomy and crest; (G ) achieving primary closure; (H ) periapical radiographs for the dental implants placed at the right maxillary molar and 1st premolar sites with good parallelism, as seen by the implant carrier with additional bone graft into the sinus cavity, as revealed by the dome-shaped radio-opacity.
References
-
Potential risk factors for maxillary sinus membrane perforation and treatment outcome analysis. Clinical implant dentistry and related research. Volume: 21, Issue: 1, 2019 - Saša Marin , Barbara Kirnbauer , Petra Rugani , Michael Payer , Norbert Jakse
-
A simplified classification and repair system for sinus membrane perforations. Journal of periodontology. Volume: 74, Issue: 10, 2003 - Paul A Fugazzotto , James Vlassis
-
Assessment of the effectiveness of platelet rich fibrin in the treatment of Schneiderian membrane perforation. Clinical implant dentistry and related research. Volume: 19, Issue: 6, 2017 - Elif Öncü , Esin Kaymaz
-
An innovative technique to manage sinus membrane perforations: report of two cases. The International journal of periodontics & restorative dentistry. Volume: 35, Issue: 3, 2015 May-Jun - Giampiero Massei , Federica Romano , Mario Aimetti
-
A paradigm for evaluation and management of the maxillary sinus before dental implantation. The Laryngoscope. Volume: 128, Issue: 6, 2018 - Yi-Wei Chen , Fu-Ying Lee , Po-Hung Chang , Chi-Che Huang , Chia-Hsiang Fu , Chien-Chia Huang , Ta-Jen Lee
-
Repair of a perforated sinus membrane with an autogenous periosteal graft: a study in 24 patients. The British journal of oral & maxillofacial surgery. Volume: 56, Issue: 4, 2018 - H A A B de Oliveira , R P F de Moraes , P H J O Limirio , P Dechichi
-
15-Year Retrospective Study on the Success Rate of Maxillary Sinus Augmentation and Implants: Influence of Bone Substitute Type, Presurgical Bone Height, and Membrane Perforation during Sinus Lift. BioMed research international. Volume: 2023, Issue: , 2023 - Vanessa Helena Jamcoski , Fernanda Faot , Raissa Micaella Marcello-Machado , Ana Claudia Moreira Melo , Flávia Noemy Gasparini Kiatake Fontão
-
Postoperative perforation of the Schneiderian membrane in maxillary sinus augmentation: a case report. The Journal of oral implantology. Volume: 40 Spec No, Issue: , 2014 - Kyu-Hong Jo , Kyu-Ho Yoon , Jeong-Kwon Cheong , In-Seong Jeon
-
Evaluation of Different Approaches for Sinus Membrane Perforation Repair During Sinus Elevation: A Systematic Review and Meta-analysis. The International journal of oral & maxillofacial implants. Volume: 39, Issue: 1, 2024 - Lélio Fernando Ferreira Soares , Carolina Mendonça de Almeida Malzoni , Marcela Lunes da Silveira , Elcio Marcantonio Junior , Suzane Cristina Pigossi
, -
A novel technique to close large perforation of sinus membrane. ORAL & implantology. Volume: 6, Issue: 1, 2013 - M Clementini , L Ottria , C Pandolfi , P Bollero