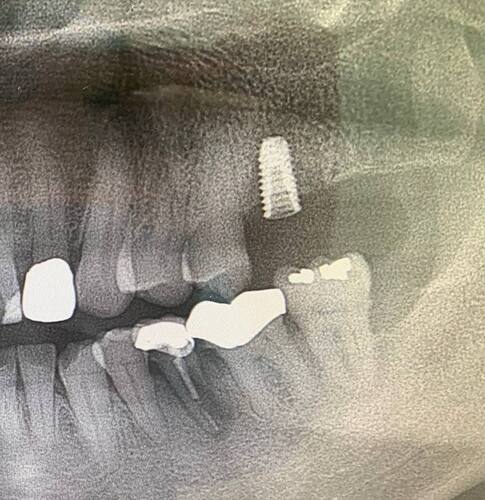
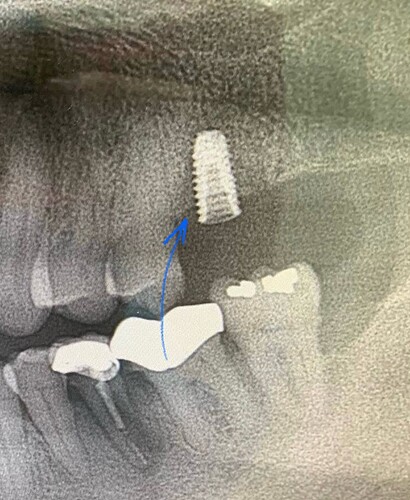
This implant 5.0x10mm was placed a few days ago. Due to inexperience, I was unable to get it down the last 1mm even after hand torque. Implant was initially at 30-40N torque but eventually was 15N after my attempts to hand torque it further. Ended up placing a cover screw and closing up for a stage 2. The X-ray shows the implant supra-crestal. Am i still able to restore this? Patient has a thick gingival biotype.
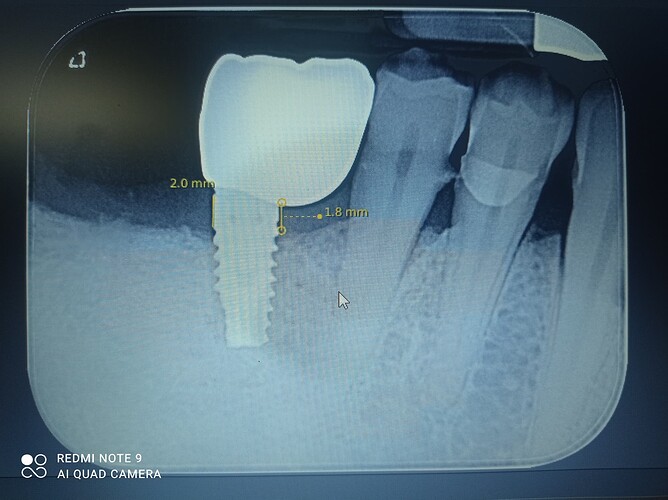
Yes and as a general rule the maxilla is much more forgiving in this regard because, generally, there is thicker soft tissue covering the ridge than what is usually present in the mandible. The loss of insertion torque after the multiple attempts is likely the result of stripping out the threads within the soft maxillary bone. I assume that you used a static guide rather than conventional surgery which kept you from being able to visualize the ridge… In this particular case I would be more concerned about the lack of interarch/restorative space than I would about the potential of an exposed collar and the inability to fully seat your fixture has cost you some valuable restorative space.
Thanks for the advice @scotty, my inexperience probably led me to either not drill to the adequate depth/ did not enlarge with the cortical drills during the osteotomy. To compensate for the restorative space, I will have to fabricate a screw retained crown.
From the description, it sounds like you stripped the osteotomy when attempting to further torque the implant. A mm or so supracrestal is typically fine, but with the amount of supracrestal height here the likelihood of peri-implantitis is high for this implant - especially so if the biotype is not super thick. I think the best options here are to replace the implant with a larger diameter than the previous osteotomy or take the implant out, graft the site and reattempt implant placement after graft healing.
This is sort of an antique solution but I used to have my residents place parallel walled fixtures into an osteotomy intentionally prepared 1mm longer than the fixture being placed. This would allow them plenty of wiggle room to properly seat the fixture into its final position in relation to the ridge and surrounding soft tissue. I still do this when I place a tissue level fixture because the final margin is built into the fixture and I like to allow some forgiveness to fine tune the placement. This solution is of limited value though when using tapered fixtures because trying to fine tune within a tapered osteotomy with a tapered fixture will bore it out and result in a loss of insertion torque, just like you experienced. I have always felt that a person should perform at least 50-100 implant placement surgeries via conventional surgery before they resort to fully guided and/or flapless because while CBCT is a wonderful tool it is far inferior, IMHO, to direct visualization and palpation of the structure being manipulated.
Fully agree with Scotty’s advice advocating extensive conventional surgical placement experience prior to moving to flapless protocols. It builds a working knowledge of anatomy and a “feel” for the bone.
It is good that you are reflecting on the procedure to try and improve. An obvious point here is that there is so much more depth before you hit the sinus floor that once you were stuck at that level or didnt have enough torque, you should have removed the implant, prepped deeper, and placed a longer implant with adequate torque at the appropriate bone level. Using a wider implant is also an option although it would depend on how wide the ridge actually is which cant be observed here.
This implant is “restorable” for sure but that’s not saying much. In my opinion, best practice at this point would be to replace the implant before proceeding to the restoration.
The elephant in the room- why didn’t you take an X-ray, realize you were short, remove the implant, drill deeper and place again? Why are you compromising long term success for short sightedness? Tell the patient you just aren’t happy with the placement, back it out , re- prep and place new longer implant. Then you don’t need to worry about your exposed threads- more than 1 mm- and you can begin the case with a higher level of comfort. Since these are basic implant tenets, I encourage you to take a Maxi course, implant pathways or another training method like Kois to be more in control of future cases.
Hi, it is best to remove and replace, this fixture will definately result in crestal bone loss, cratering, and a poential law suit and bad reputation. At thestart of my implant journey 20 yrs ago, I placed a fixture with exactly the same situation, well enough, it failed 5 years later. Explain to the patient you are not happy with this restoration as you want this to last as long as poss/your standards are higher etc etc, and DO NOT CHARGE again, a good patient will understand you have their best interest in mind and appreciate the effort. Don’t kick yourself in the teeth, this stuff happens to experinced surgeons, just own it and do the right thing, it wil make you feel 1M $$$. Wish you all the best
I agree with you that this is not ideal and in a perfect world should be removed and replaced but could you please explain how this supracrestal conical connection with the microgap medialized and above the crest can have such a predictable and catastrophic prognosis??
There is 2-3 threads exposed. So, you would still want to proceed with restoring this? The other option is to remove it now, re-prep deeper, and place and bury an implant and set it up for long term success
There’s quite a bit of bone loss on the mesial, if you try to restore this it will fail very quickly. Remove and replace 4-5mm deeper.
I think your drill not deep enough, from my experience sometimes its hard to see the depth marker on the drill when its covered with blood, its more easily to use drill stopper, i suggest you to remove the implant and drill with wider and deeper drill
If you restore it maybe it will survive 1-2 years, but after that it will fail and you need to spend more money for bone graft, membrane, new crown, new implant etc…
Since the individual who originally posted this is, by their own admission, new to implant dentistry I think it is best if you/we don’t fill him full of false information. While this fixture may very well fail at some time in the future there is no bone loss on the mesial. Bone loss would imply that it was lost since the placement of the fixture and in this case it was never there to begin with as the screw was just not placed deep enough. While we all have different opinions and techniques related to the craft I don’t think that a false statement like this is helpful to the person trying to learn from their mistake.
I had an experience similar to yours. one of my first surgeries so I tried to restore it. For 5 years the patient had no problem but suddenly the patient had pain when chewing. I had to remove the implant and redo the work.
@scotty I think the main question right now for me would be:
- leave the implant + restore, keep the patient on a regular maintenance regime with good oral hygiene to reduce risk of peri-implantitis and monitor, manage complications when they arise
- remove and replace the implant, but requires another surgery/ bone grafting procedure
I would think the biggest risk here to implant failure here would be Peri-implantitis in the long term
I see, yup looks similar. was the failure due to peri-implantitis?
I think we can all agree that it is not an ideal situation but it has the advantage of being in the maxilla and, per the doctor, has a thick biotype. This thick connective tissue covering is, IMHO, a critical factor in maintaining peri-implant health so I think it is reasonable to assume that this should/could behave differently than a similar situation in the mandible or any area covered by thin mucosa. Thick overlying connective tissue is probably more important to long term implant, and teeth, stability than the bone support and a lot of research within the ITI (International Team for Implantology) is starting to focus more on this. In other words thick tissue protects the bone and this shallow fixture in the maxilla has a better soft tissue barrier than the same shallow fixture in the mandible.
If you look closely at the periapical, there is a radiolucency running up the mesial of the implant. The periapical is grainy, maybe the original poster has a better or more recent image, or probing depth? To me, it looks like it’s losing bone. Even with a thick biotype it’s hard to imagine that there is more than one mm of tissue over the implant platform. This does not satisfy the biologic width needed for crestal bone stability. Because the poster is admittedly new to implant dentistry it’s very important to give accurate information based on science. That’s what I’m doing. Telling him that it will be fine is bad advice.
The image he posted was taken the day of the procedure… it is impossible for peri-implantitis to occur within minutes.