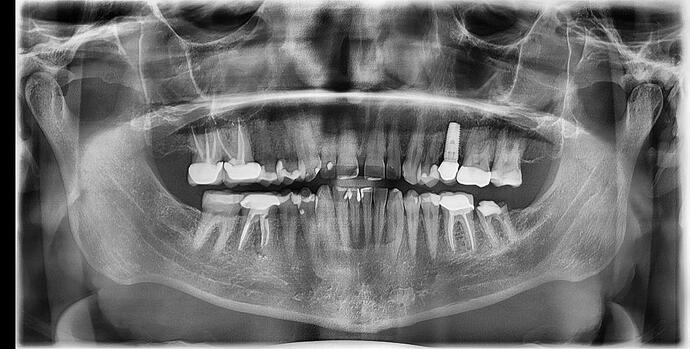
That radiolucency that you refer to is most likely the result of him wallowing out the osteotomy as he tried to hand torque it further…by actually reading the original post I am able to gather the facts surrounding this particular case rather than just being critical of the final result. If you look closely at the PA you will notice that there isn’t even a cover screw in it and if you read the post he states that it was just done a few days ago. These two pieces of information are enough to tell me that the image was taken way too soon after placement to accurately asses the “bone loss”.
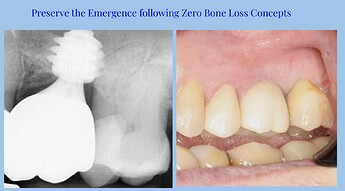
We need 4mm of tissue between the free gingival margin and the platform of the implant to satisfy the biologic width requirement and to get crestal bone stability. The implant is at least 2mm supracrestal, that means that the patient would need 6mm of tissue thickness over the crest, which is super unlikely. Big complications happen when we ignore small complications. This is not a big deal to fix. Tell the patient that you don’t love it the way that it is and that you would appreciate it if they would let you try to get a new implant in better position. Then if they allow you to, I’d go a good 4mm deeper than the current implant, which should put you 2mm subcrestal. You will need to profile the bone a little bit to allow for proper emergence.
If you leave that implant, you’ll regret it every time the patient comes in for hygiene with inflamed tissues of peri-implantitis. If restored as it is, there’s no room to build the proper emergence, so you’ll end up with the dreaded Tomato on a stick restoration that will be a food trap. Food traps lead to peri-implantitis. It may last three, four or five years until it eventually fails, but then you will have a much bigger defect to deal with.
You are right, I didn’t realize that the X-ray was immediately post-op but that doesn’t change one word of my response. This implant is way off where it needs to be and should be removed.
This is from an immediate placement that was done today. One rule of thumb for placement depth (for conical connection) in molars is to get the platform level with the furcation of the adjacent molar. This allows for development of proper emergence so you don’t have food trap issues. It also contributes to crestal bone stability when we have at least 4mm of highly polished Zirconia against the tissues.
if you just placed it a couple days ago. i would just have pt return. remove implant. drill 3-4mm deeper and place the same implant you dont need a new implant at the correct dept. either equicrestal or subcrestal. you are atleast another 6mm from the sinus floor plenty of room.
not a big deal at all. just osteotomy deeper and torque down the same implant. with the correct drills you should get 35Ncm torque again. no bone graft needed.
you over torque it. that probably why your torque dropped to 15Ncm. over torque can cause bone necrosis. good luck.
dont leave the implant like that. not a big deal. drill deeper. you already have a hole. work is half done.
if implant placement is a 3 dimensional task, based on your X-rays, we do not know the Bucco-lingual placement of it. You can take picture of it’s placement occlusal, to know if it is positioned in the comfort zone.
Positive factors of influence in this case:
Maxillary molar tooth, possible low esthetic risk
In general lot of keratinized tissue
As reported thick pheno type
Negative factors of influence in this case
Bone level type placed as a tissue level
if the surface roughness values are higher, you will have mucointegration issues
Unknown factors of influence ( at least based on the info provided)
Technical complications- When the implant is loaded ,it’ s a different beast to deal with.
rounding up : you have biologic complications, and technical complications down the road.
how do you manage it ,
As per ITI: PROM, patient related outcome measurements,
address the situation with patient and see where it goes, monitor now under loading for now and deal with the problems later
or
re-do it now
Recent ITI Singapore Symposium buzz words were:
bone sets the tone
tissue is the issue
prosth is the boss.
Hope this helps
It is easy to remove now. Just back it out. When you do, improve surgical access for better visibility and take pilot drill film to confirm position. Go back to basics. You can use The same implant or go longer, but be sure to undersize the osteotomy. Do not fret. We have all been where you are. But better to make the correction now than after the case fails or is even more of a challenge to restore. Proper position will give you additional room to restore. I would also correct the supraruption of lower molar at that time.
I am stunned that anyone would coach a novice to accept this result. The rough implant surface that will be in the sulcus. is a nidus for bacteria. The best way to do top notch dentistry is to correct mistakes as soon as they are made. Then we don’t repeat them. We ALL have made this and countless other mistakes. If you back it out, drill deeper, you likely can place another fixture all in the same surgery.
This is from a lecture I gave for MegaGen at the North American Scientific Meeting in San Diego in October. The title was Molar Immediacy and same day 3D printing. The above is three year follow up for an immediately placed and immediately provisionalized site. The platform is a good 7mm below the free gingival margin and there was running room to develop proper emergence and get a good tissue seal with mirror finished Zirconia against the tissues. Bone is right up on the platform of the implant. We get these kind of results in a highly predictable manner when we follow some basic concepts.
Bone loss and remodeling are not inevitable. It’s completely preventable when you pay attention to all the little details.
You are absolutely correct and it has unfortunately taken me years of experimentation with multiple products to come full circle back to Tissue Level (Straumann TL) fixtures. Oddly enough every modern concept of conical connection/platform switching/medialized abutment is done in an effort to replicate the bone preserving nature of an antiquated fixture design dating back to the 1980’s. Place a tissue level fixture with the surface treatment in bone and the physics of the simple design will take care of the rest… Or we can place conical connection fixtures Xmm subcrestal with various configurations of different transmucossal healing components on top of universally undersized platforms. The end result is the same!!!