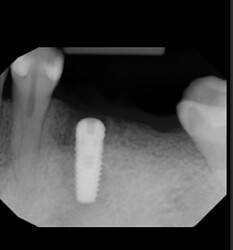
Hi just placed an implant with torque 15 ncm. I have recalled patient after 4 months. Will this implant fail because of low torque? Should I remove this implant now instead of waiting for 4 months ?
no problem. what you have is a spinner. keep the implant buried. I’m sure it should integrate. check in 4 months with a PA. as long as there is no radiolucency you should be able to do a 2nd stage. nothing wrong with waiting for integration. i’ve placed plenty of spinners,waited for integration and end up with a stable implant.
Thanks for your reply
Not a problem at all in fact it might actually be better off and more likely to succeed. Prior to All-on-X it was normal to place a parallel walled implant at 10-20Ncm with or without a transmucosal healing abutment and the results were at least as good. Personally I have had very few failures with fixtures placed at low torque while the majority of the failures I have seen have been with fixtures placed >40Ncm. Considering that most of the posterior fixtures that I place are parallel walled tissue level I routinely insert them at 15-20Ncm and with the 1.8mm transmucossal collar and the 1.5mm cover healing cap I am essentially placing a 3mm healing collar on these “low torque” fixtures and sleeping just fine at night. I strongly believe that primary insertion torque is the most overhyped and false sense of security promoted in implant dentistry and the success of Straumann dating back to press fit cylinder fixtures is all of the proof that I need to discount the importance of insertion torque. You will be fine…
Your information and guidance always helps. Thanks a lot
We have a poor PA (threads fuzzy), so hard to see what that radiolucency is from or read HU. The reason it will fail is force factors. Where is the implant behind it? Why isn’t it 1.5mm from the adjacent tooth? What is your plan for managing the chewing forces? When you have a question to ask, be cognizant of the fact that the better the information you give the better the answer. Where is cross sectional CBCT, Did this perforate the buccal or lingual cortical wall? Was this recent to extraction and S.G.? Why wasn’t 19 placed at the same time? You need 3mm between implants, 1.5mm from external wall to adjacent tooth. Do you have a virtual crown you have placed for 19,20 on a cross sectional image? These are things that if planned properly will aid in your future success. Lastly if the HU is so poor, you need to undersize your osteotomy so you dont have a spinner as a lot of spinners do not integrate. And if this one does your force factors are magnified by not having a plan for 19 and restoring it at the same time. See misch 3rd edition Contemporary implant Dentistry.
Tooth was extracted 4 months ago and thats why the radiolucency is present . Implant is 2 mm subcrestal and well surrounded by bone on all sides. Soft bone protocol was followed and osteotomy site was under prepared.No buccal or lingual plate perforation was done . Patient was explained about 2 implants but denied because of financial reasons (may come back in future for that).
Thank you!
Dear Dr Ninja
You may be an implant warrior but how about taking it easy on a colleague with all your criticism. He may be in the embryonic stage of his implant carreer but there is no need for your tone.
Agree that his approach is certainly not helpful and of questionable value…
the PA is fine. i can see the threads just fine. its white all around the implant which is good. you will know if implant failed. it will have a nice dark halo around the implant. which ive seen plenty. also 1.5mm is recommended minimum. doesn’t mean it can’t be 2mm or 1mm from adj teeth. the implant isn’t placed that far off. not every office has a CBCT and 3D printer to print surgical stents to place perfect position. ive done plenty of implants with just PA or PANO. and the implant and crowns r just fine and lasts >5 years. why isn’t 19 placed same time? most likely patient dont have the funds. can only do one implant every 2 years. i literally have patients who do not want to pay out of pocket and do each stage once a year. very frugal patients. actually, when torque is high you will get pressure necrosis and like dr scotty says which i agree and encountered sometimes. higher torque has higher failure rate than less torque. implant failure is not a problem. you will encounter implant failures when you placed enough implants. its part of implant dentistry.
Excellent description and so much more helpful and less arrogant than that of Ninja… Feedback like this can actually be helpful unlike the criticism dealt out by an individual who spews bullet points from a textbook. Thank you!!
Thank you for your reply. I will update with a new cbct and a pa after 4 months.
i can be arrogant and snobby also. but we all here to learn and get better for the sake of our career and patients. only our patients suffer when we are inadequate in our skills. dont even waste time on post op CBCT on a single implant. im sure its pretty straight. it looks fine on the PA and that’s more than enough. im sure your lingual/buccal distance is fine. luckily implant position is a range, not absolute. just tell us after 4 months when you do a 2nd stage the implant is solid or mobile. if PA is white around implant. just do a 2nd stage. sometimes for posterior. i do 2nd stage and PVS impression same time. save chair time. see how lazy i am.
Thank you for your explanation!
While some colleagues think my tone was abrasive, I wouldn’t have taken my time to respond if I didn’t think I was imparting important information. I have undergone training in many Implant organizations and it is an excellent source of mentorship. The points I am bringing up are very important. First, a non-parallel x-ray is not diagnostic and would not stand up in court. Threads of the implant are blurry so this is not an angle that can be read properly. Next, just because a patient cannot pay for two implants does not obligate you to do 1 and have it suffer due to increased force factors. This implant which is already potentially ailing/failing will be subjected to higher chewing forces by not having an implant or tooth next to it. In my practice, I would have the patient save up and do both implants at one time or postpone and I would explain the risks of proceeding with one implant. I have seen many implant failures and I believe this dentist-needs a mentor that can review these things before simply placing an implant. (If you were to include a software image of 2 well placed implants virtually, it would show that proper measurements were made prior to osteotomy.)Yes it may come across as arrogant-but it really is not arrogance but concern for the patient and the dentist. Proper planning will allow this dentist to improve their technique and planning. Also to request proper advice without a CBCT cross sectional image is inadequate. I certainly hope this implant works out. But if we are to give young dentists information they can use, it can sometimes require real advice, even if it may hurt their feelings a bit. I suggest this dentist take courses from the AAID, Resnick, Implant Pathway, Maxicourses, etc. and have some mentors to help on their learning curve.
By the way, sequencing dentistry due to lack of funds is excellent —except where it may compromise the end result. Feel free to read my articles on Upgradeable Dentistry at www.hamptondentalassociates.com But for one doctor to blame placement or say some people cannot afford a CBCT is not ever an excuse. I refer my patients for their CBCT for every case I do. CBCT is standard of care for implant placement. My scans are uploaded in 24 hours and I can plan everything regardless of if a guide is used as many implants can be placed free hand if desired. I wish you continued success.
Sincerely,
Richard Winter DDS. MAGD, DICOI, FAAID, DABOI/ID
Master Academy of General Dentistry
Diplomate International Congress of Oral Implantologists
Fellow American Academy of Implant Dentists
Diplomate American Board of Oral Implantologists/Implant Dentists
Dear Dr Ninja,
Just because you have more letters than the alphabet after your name does not
impress me nor anyone who reads these threads and posts. You may be a Master, a Diplomate and a Fellow but you still have a long way to go in the humble and humility department. Why don’t you look in the mirror for a moment and come down from your high horse. You might learn something.
I have found that when people boast of that many letters behind their name there is usually more to the story. I bet if those letters are unscrambled then they will spell out the story of a kid who rarely made it to school without having their lunch money stolen… so sad…
OK. i admit you have lots of credentials which you paid to add behind your name and also have enough success to prove your proficient in implant dentistry. That does not negate the fact that the placement of dental implants is a procedure, not a National Certifying Boards for Dental Specialists (NCRDSCB) recognized dental specialty. Dental implants like all dental procedures require dental education and clinical training. like everything in dentistry. Implants does not last forever, and no one is 100% successful in implant placement and restoration. Just because you have lots of credentials does not make you a dental implant specialist. because none of us are dental implant specialist.
I assume you run a high-end office which you only treat patients who can afford your rates and implant placement on optimal conditions. unfortunately, not all dentists have the luxury of having a CT in house or close by or every patient willing to pay for CBCT scan. Nor does every dental implant placement need CBCT. I know you think CBCT is the standard of care. BUT LEGALLY CBCT is not a standard of care in Dentistry. Please read ADA ISO 16498:2013, Dentistry — Minimal dental implant data set for clinical use. or ADA Standard 172. While we all want CBCT before and after implant placement. Thats just not a realistic requirement and ADA understands that and given dentist flexibility. Just like PANO is not a standard of care in wisdom teeth extractions. I can use PA as long as the whole tooth is on the PA. But PANO and CBCT definitely helps in treatment planning and procedures.
you probably only cater to high end celebrities which money is no objective. But most of our patients do struggle with finances but still want to have implant treatment. Patients are willing to buy car, purse, shoes, jewelry, cell phones, etc. but considers teeth secondary to their materialist desires. Even though teeth should be their top priority in expense since they use their teeth 24/7. lots of my patients drives benz, Porsche, Bentley, etc but haggle with me all the time. You are lucky you have a good front desk/office manager/treatment coordinator which helps your patients with finances to complete their treatment with you.
You are not hurting feelings. I think your critiques are all valid and are textbook examples and principles. I am assuming Dr Jdent have completed some form of dental implant training including hands on training. I doubt any dentist would have enough surgical experience and bravery to place dental implants with zero training.
some of my patients only want implants to replace missing teeth. even though rest of their natural teeth are in terminal condition. They simply won’t listen to a dr’s advice to remove all their teeth or have the funds to do a full mouth rehab. Sometimes. they only want to do treatment in sequence even though the treatment is compromised and not optimal/ideal.
In an ideal world. all dental treatment is covered and i can plan, treat and bill any dental conditions treatment the way i want and all patients agree to my treatment plan. if only life is that simple. but requiring patients and putting down doctors to follow absolute requirement to have CBCT and perform all treatment in unison is just unrealistic.
Just in case you forgot even with all the CAPS behind your name. You are still a GP like me. ![]()
I think I will start referring to myself as Dr. Scotty, DDS, BAMF, Diplomate of Common Sense and no BS, Board Certified Tooth Mechanic… maybe with these extra credentials I can become so important
i dont think Dr Jdent is b u t t hurt. but constructive criticism is more beneficial than just criticism. Im sure if Dr Jdent have more friends to ask. he would but he’s asking us out of humility and reassurance. Which i can definitely resonate. implants are not even challenging for me anymore. But I love challenging GBR cases. in fact im working on a huge GBR case. a pt with h/o ameloblastoma resectionx2. Even Dr Scotty questioned my aggressive treatment plan. But i need professionals to question me so i can justify or alter my treatment plan. There’s many ways to skin a cat i tell patients. Thats why the 1980s readers digest article regarding dental treatments really put dentistry into scrutiny.
we all want to get better at any stage of dentistry.
Just bc we are GP doesnt make us any less capable implant surgeons than specialists. In fact i wish some specialists would stop placing implants. I had 2 refer me patients they placed a mouth full of implants and tell me to restore. I had no idea what happened. but i have to figure out how to restore them.
Since most specialists dont restore implants. they dont consider how difficult it is to restore poorly positioned implants. they assume GP can figure it out with custom abutments and angled abutments.
So just bc im GP doesn’t make me less proficient than specialist and vice versa.