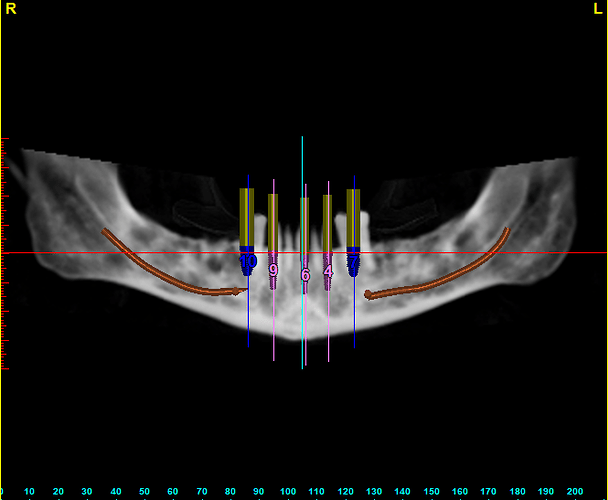
My patient is a 55 year old male who was in good health prior to implant placement on the lower arch. Extractions and bone grafts with immediate lower denture was done. A few months later the patient was hospitalized and had open heart surgery to repair an aortic valve and stents placed for coronary disease. He is currently on daily aspirin, plavixx and antibiotics forever according to his cardiologist. It has been six months since the heart surgery and his cardiologist has cleared him for dental surgery with the following precautions. He must stop the plavixx for one week, the aspirin for 5 days and antibiotic prophylaxis for the valve replacements. My question to the community is how would you continue with this case? More specifically would you continue with implant placement? If so how many at one time or split up the quadrants into separate visits? Also limited amount of vasoconstrictor that can be used so how would you manage local anesthetic? See attached preop pan. Thanks
These are all great questions relevant to the surgical planning. The vasoconstrictor question must be answered by the cardiologist. Considering the “pre-operative protocol” in terms of holding his blood thinners, I would recommend completing all of the surgery in one visit to minimize the number of times the blood thinners would need to be stopped. From your pre-operative CT image, this looks like the implants could have been done at the initial surgery. It is interesting to note that in retrospect considering the unpredictable cardiac event he had. Good luck with the case. Let us know how you handled it.
I would approach this as a single visit case for the surgical aspect. I agree with drdangober that holding the blood thinners repeatedly might not be the best thing to do in the patient’s interest. If patient can be sedated (moderately or even with general) it might help you manage intraoperatively much better and you might be able to complete the procedure sooner. Good luck with the case.
Being a contrarian, I would hesitate to stop the aspirin nor the plavix prior to implant placement but rather discuss it more with his MD. A quarter carpule of 1:50,000 xylocaine infiltrated at the surgical site on the ridge only, should be discussed and concerns for bleeding. Antibiotic coverage can also be discussed in more detail and perhaps just given the day of surgery.
Minimally invasive surgery should be considered for your case , maybe navigated or guided or flapless?
Good luck!
I’m surprised that in this day and age, that blood thinners are being “held”. 16 years + ago the cardiologists concluded that the risk of a stroke or heart attack, is much greater than bleeding out. In this case if you immediately load it, the PFCD will act as a band-aid. Ask a physiologist about epi/adrenaline or go to an American Society of Dental Anesthesia meeting and ask a speaker. Our bodies put out more adrenaline than what’s in our local anesthetics. If they feel pain, then they’ll put even more out. I’d use carbo to start and then immediately add Marcaine with 1 to 2:00,000 epi. This also works well for patients that tend to get palpitations. Bleeding in these patients can be easily managed.