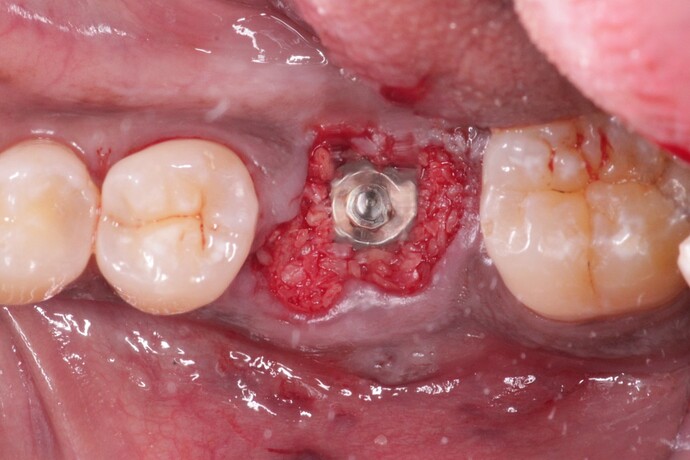
Different surgeons feel differently about the need for a membrane over the socket of an immediate implant and bone graft when NO flap has been reflected. How do you approach this in your practice and what is your rationale? Look forward to hearing your thoughts.
Exactly like this!!! I would approach it this way even if a flap were raised and the buccal plate were compromised because it is a contained defect and even in the absence of a buccal plate would still have 3 walls. I have done this, without a membrane and often even without a graft, for the past 12+ years even back when the rest of the implant dentistry world was convinced that a teflon membrane was necessary to utilize and remove 3 weeks later. The point is that the graft is nothing more that a matrix to help stabilize a clot and in the presence of bony walls for containment their is no rational explanation for the use of a membrane. Great topic for discussion…
what holds the particulate in place in this example just the blot clot ? Wouldn’t it wash out with no flap or membranne coverage ?
I agree with previous post??
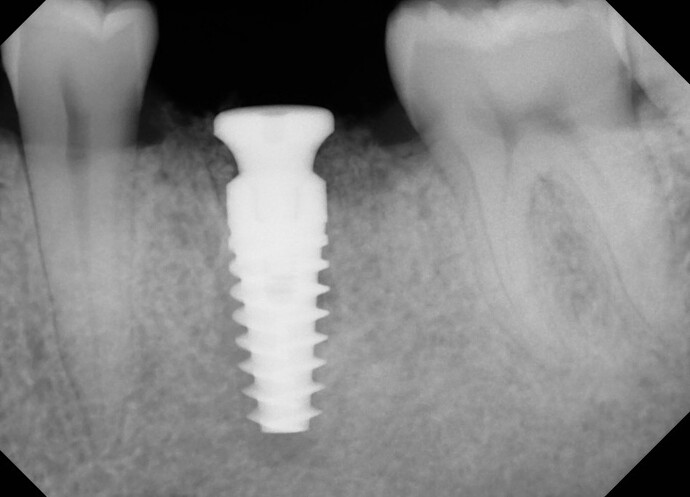
In a molar site I generally don’t place an immediate implant. Rather I do the extraction, allow around 3 months socket healing and redevelopment of gingival closure over the socket. I then place the implant in native bone without a graft and I can be sure there will be plenty of keratinized gingiva all around the implant. The molar immediate implants I do place work fine but the incidence of exposed threads above bone is greater for these cases.
The answer is “don’t worry about it” because all you see is overfill which doesn’t need to be there in the first place. In spite of our best efforts at screwing up Mother Nature with artificial osseoinhibitors extraction sockets have been healing quite well for centuries so this is more than enough intervention. The nice thing is that there is no wrong approach, membrane vs. no membrane, but rational justification for the use of a $500 additional procedure to place a membrane is not available when the defect is a 3+ walled extraction…
I understand your rationale but my experience has been to place a molar immediate whenever possible as I have had great results. I will frequently, at no additional charge to the patient, simultaneously augment the soft tissue via a connective tissue graft as it is simple and provides a much more justifiable service that any osseous graft could ever provide to a fixture placed within the confines of the walls of a fresh extraction.
You could just put 1-2 interrupted sutures over the top and will will close that supracrestal gingiva right over the grafted area… or you could place a couple of drops of cyanoacrylate/super glue over it. Either way it is easily addressed if you are so inclined as to worry about it. I would suggest stopping short of an additional billable procedure
You’re right. Many different approaches will work. What we become accustomed to and comfortable with in our practices is what we as individual practitioners tend to provide our patients. If it works in our hands we carry on. This is one reason this forum and the AAP Open Forum are so interesting to follow. We are able to see how others do things in their offices.
It is interesting to see that immediate molars are still not a preference for some clinicians. It is definitely a routine part of my practice. When I was training in residency, we placed a lot of immediate implants and we would often discuss how as long as the conditions for predictable socket healing are present then we can be “confident” in the success of the procedure. I vividly recall Dr. Sigmund Stahl putting up a histology slide of a healing socket with bony projections coming from the socket walls towards the center and asking, why wouldn’t this work with an implant stuck in the middle? That always resonates with me.
To me, the question boils down to the following- do you need to grow bone in order to facilitate proper positioning and insertion torque of the implant? If so, then clearly immediate placement is not a good idea. But if not, then it can (and should) be a consideration.
Thanks everyone for the valuable discussion!
great question- that’s what this post was getting at. Typically the blood clot will hold it in place. Surgifoam or collagen tape can also be placed if one is not comfortable with this. To me, elevating flaps/tissue to place a membrane in these cases seems superfluous and could even work against us by compromising some of the blood supply of the periosteum.
Newer ‘form-stable’ grafts and sealing technologies have emerged that suit this indication. There are several brands available in Europe that firm up in the defect and do not need a membrane for containment. One example is Powerbone Dental Putty. Because no membrane is needed there is no need to extend a flap with the ease and healing benefits this brings. The open site can then be sealed/protected with something like Ora-Aid which is CE and FDA approved.
Link to Powerbone Dental Putty after this for those interested to see more. https://restore-surgical.co.uk/offer-powerbone-dental-putty/
Can you please explain what you mean when you say “no membrane is needed”? Are you referring specifically to case like the one above or in general?
In general.
The main reason for a membrane is containment of the mobile particulate graft. Form stable grafts are self supporting so do not have the requirement. Some will say theyvuse a membrane as a barrier for invasion of soft tissue albeit that this soft tissue is more likely scar tissue that would otherwise form due to micro movements on the surface of a mobile graft.
With an immediate in these situations I like using a temporary abutment (like a peek) and contouring it with flowable composite to the edges of the crestal tissue and controlling your emergence profile. As long as you have good primary stability and you keep it way out of occlusion - I’ve had good results.
I did, along with a former resident mate of mine who is now a perio program director, a sort of case series in which we used a laser on coagulation mode and no graft. Our protocol involved extraction and debridement of the socket in order to promote bleeding. Once sufficient blood flow was established we would coagulate the blood filled socket using the coagulation setting (4.2W, 600microsecond pulse on the Millennium Periolase) and allow the site to heal for 6-8 weeks prior to implant placement. During my perio residency I was fortunate enough to work with some extremely good clinical research clinicians and the overwhelming conclusion is that the graft is nothing more than a clot stabilizer and the presence of a stable fibrin clot is all that is needed. I can tell you that I have done this literally hundreds of times and today I still do it though I don’t even bother with the laser as pressure on a clot is all that is needed. Interestingly enough my friend ended up publishing this although he used a graft in the publication simply because it was seen as more interesting to the reader because we dentists love to use extra stuff… Bottom line is that the graft in a socket is just feel good thing and its only purpose is to assist in clot stabilization
This was my first true exposure to what I like to refer to and have been criticized by the administrators of this site for using the term “Made for Publication Technique Article”. It was “more publishable” to unnecessarily use a graft as that is what the reader wants to see. Still nothing wrong with using a graft I would just be careful claiming that it is necessary…
yes, that is an excellent way to manage these extraction sockets and maintain the natural emergence profile. Thanks for sharing.
Thank you for clarifying. But in general, I don’t believe the main reason for a barrier membrane placement is for “graft containment”, at least not according to the way it was discovered and researched in the literature. I would be interested to see clinical examples showing the success of the grafts if you have any available. Thanks for sharing!
@tcperio Trust me, you are preaching to the choir. See my article about this exact concept. Flapless Extraction Socket Healing Around an Immediate Implant Placed into a Mandibular Molar Site Without the Use of Regenerative Materials: A Case Report - PubMed
But I would not go so far as to say grafts are simply “feel good things”. Study after study has shown that they contribute to the dimensional stability/preservation of the overall ridge contour. I would prefer to say that the blood clot is what is responsible for the actual healing of bone and integration of the implant but that the bone graft increases the likelihood of maintaining ridge dimension (when used correctly in the right situation). Great discussion.