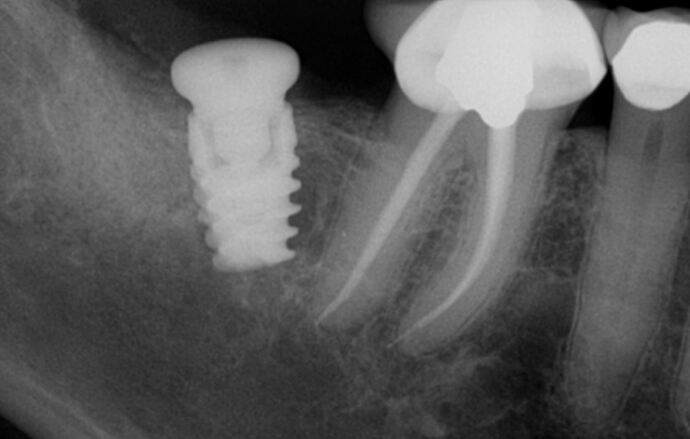
I misangulated this implant. I was debating whether to remove, graft and redo it. Is this case fine to be restored (from a surgery student’s standpoint) ? What do you think? Would you have removed it, grafted and come back? Would you still remove it? Aside from doing a better introperative xray checks to ensure better angulation. Thank you!
I’d explain your possible concerns and procedures required to remove etc and allow patient to decide - most would prefer completion with the undertaking that IF removal required at a future time (say 3-5 yrs) you’d do so at no charge (appears integrated- how long ago was placement?)
Will be difficult to restore and maintain. Remove as soon as possible
Patient is not the one that need to decide if it is wise to keep it. Removing it is the good choice. Thanks
Tricky one. A good time to reposition would have been at time of placement. You’re almost parallel to premolar. Molar, not so much. I have restored a bunch of these and haven’t had much issues. 2nd lower molars are a tough site. More likely to hit nerve and bone is pretty dense. I would let it heal and take it from there. I wouldn’t expose patient to recurring surgeries and bigger risks. Explain the situation properly to patient and in all fairness, less is best. With that in mind, I would tell the patient if any issues arise, you would take care of it at no charge.
Question:
is there an opposing molar?
If not , simply explant and leave it be.
If yes, then explant, wait 4-6 months, and then reposition.
This is one where you’ll have to bite the bullet
Better to redo now so your patient will have long term success and you can be proud of yourself
I will play devil’s advocate. We intentionally angle implants all the time. As long as the bone is profiled so an abutment can be seated, what would be wrong with restoring by incorporating a custom or angled abutment to idealize mesial emergence profile, relocating the screw hole, and making certain there are only occlusal contacts and there are no lateral interferences. You could also use an angled multi unit abutment. It would certainly be more textbook if it were parallel to 30. However i do not think it is too close to 30 apically and expect a good long term outcome. Why condemn it at this point and put the patient through at least two more surgeries?
Find a good dental lab, and discuss for a custom abutment, its not an esthetic area so i think its still restorable
I would prefer angled multiunit or custom type abutment.
Removal is certainly a choice although there are too many unknowns (patient age, function, immediate?, augmented?, past history and readiness to retreat)
Would you want this in your wife’s mouth? Patients spend a great deal of money for this
so they deserve the BEST that you can do…is this the best that you can do??
Restoration of this implant will create a cantilever with food trap and possibly abutment loosening or screw fracture.
I would send an impression to a good lab at this point and see what’s restoratively possible and go from there. I don’t see much issue with a cantilever effect and think a decent occlusion can be generated with only centric contact. I wouldn’t want to remove and replace the implant and I say this from the surgeon and patient point of view.
it is a no-brainer… take it out ASAP and place new implant at correct angle/location before the problem compounds.
I Should advice to remove it as soon as possible!! Graft + PRF, wait 3-4 months and repeat the procedure
I agree with everything other’s have said up to this point except that I completely disagree with the notion that it should be removed and that you should somehow be ashamed of yourself. Just like every other piece of restorative dentistry, in this or any other mouth, it is not perfect but the potential for problems when you start considering removal. graft, membrane, PRF etc. seems similar to killing a fly with a hammer. I have been at this for over 20 years and this very thing happened to me last week as I also lined my osteotomy drill up parallel with the distal aspect of the “restored” adjacent tooth/crown only to have it do this very thing. I find it interesting how we criticize the slightest misdirection when it comes to a single tooth implant yet we will put them in at 45degrees off angle and then pound our chest in celebration of adding another full arch feather to our caps. If a full arch of misdirected mess is satisfactory then surely a slight misdirection of a mandibular second molar should be fine. Just my opinion and don’t beat yourself up over this.
My apologies to all who have been critical of this case but could you please explain to me, and possibly other’s, exactly what is wrong and would thus require removal of this fixture. I agree that it could be more parallel with the adjacent molar roots but it is parallel with the adjacent (for lack of a better term) path of occlusion. In the event that an integrated or integrating fixture is removed why would it ever be necessary to graft the resulting osteotomy and by all means why must you also draw blood for PRF in such as case. If this is the worst implant fixture you ever place then I think you will be just fine…
I believe that is not a matter of the implant itself, or the bone. Is a matter of prothesical rehabilitation, emergency profile and major axis disfunction. The prosthetic crown will have to be extended to achieve a point of contact with distal aspect of the last molar. In my experience, with very good prosthetists, the managed to preform the pappila, but always remains a point of accumulation of dental plaque. Is not the end of the world. But if a replacement can be done, I Suggest it would be better!!! Sometimes the patient has a crude limitation to open the mouth big enough to work properly at the distal mandibular sites. Nothing that we could manage
Restoring this is not as bad as some say above. It is very easy to be too critical of others. I think most likely you can have a restoration on this implant which will be screw retained. Just get the occlusion right and you should be fine. It seems you have angulated your drill parallel to the distal wall of LR6 rather than parallel to the distal root. This happens often and the best way to avoid if you have no surgical guide is to use pilot drill down 5-6mm then take a radiograph. If angulation is not right it will be easy to correct then.
Amen!!! I personally don’t even believe that is is worth the discussion as it should not lead to even a compromise in treatment. I hope these folks are as critical of their own work as they are that of others because that would lead to some near perfect dentistry… which I have never seen.