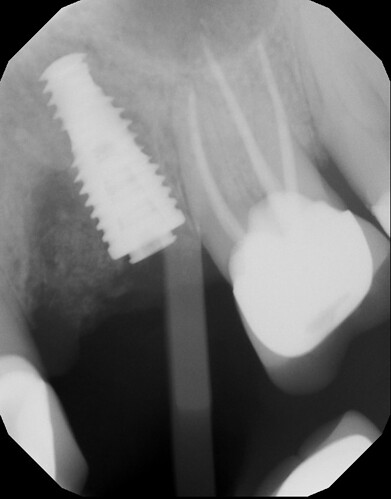
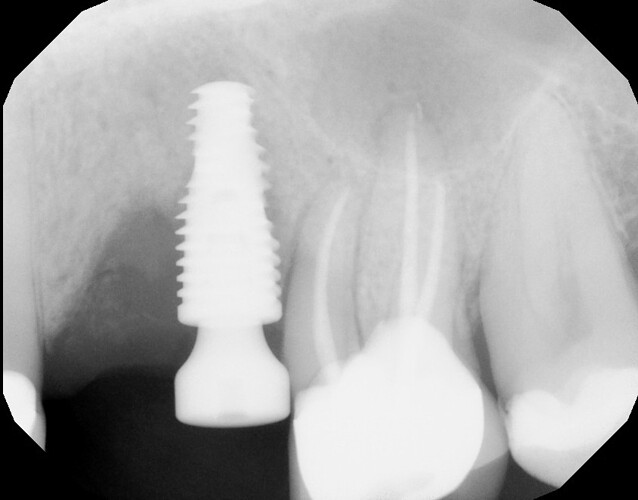
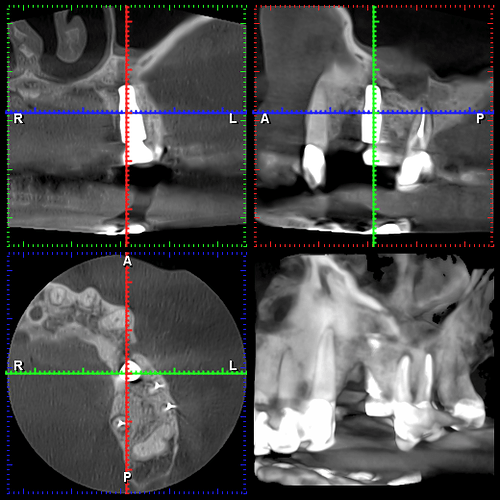
I extracted these two teeth on 3/20/23 and planned to place an implant between the two. However, I did not hit my planned mark and ended up with the implant in the #13 site as you can see but decided to leave it. I had planned and did subsequently graft around the implant although I did not raise a flap for this which I regret. Patient came in for first follow up at 2 wks (he was on vacation at the usual 1 wk follow up). Sutures were removed and healing appeared WNL. Patient came back a further 4 weeks later on 5/1/23 for a CBCT where it was discovered that the majority of graft material had been lost. No infection was noted. Implant was noted to already be “rock solid” and I decided to allow the soft tissues to fully heal an mature a bit with an option for future grafting. Patient came in for latest follow up on 6/12/23 where the CBCT pic attached here was taken. All graft material is lost. Clinically the soft tissues looked good and the defect is healed and filled with what I assume is granulation tissue. My plan is to perform further grafting, this time with a full thickness flap. I understand this to be tricky around an integrated implant so I am looking for a few tips to make this procedure as predictable as possible. Thank you!
Unfortunately, this one had no chance from the word go. IMHO, I would explain to pt that you gave it your best shot but it was not successful, remove, degranulate, graft with fully resorbable synthetic material (ethoos of Osteogen plug) and re-asses after a few months, Likely to need a block graft. It might be wise to refer to a supportive oral surgeon as the defect is now sizeable and if left can lead to loss of canine and molar.
I’m afraid that you’ll have to eat this one and explant and start from scratch
Graft the defect and osteotiomy , wait 6 months and redo
To get a predictable graft, I would remove the implant you just placed before you lose more bone on the molar, (you need a MINIMUM of 1 1/2 mm clearance with the adjacent tooth (which doesn’t show on these radiographs) and that metal won’t be friendly to growing as much bone as that defect calls for. Once the soft tissue has healed from that surgery (2-4 months) you then have several choices which I sense would all be best suited to refer: 1) GBR- 2) block graft- 3) Allograft block graft-again advanced skill. To further answer your question: Are you clear on why the implant wound up where it did? If you restore this case you will have a mesial food trap. Discuss your mistake and own it with the patient. You’ll be more likely to not have the same thing happen again. When you grafted did you use a membrane? Did you tac the membrane in place? GBR is straight forward when you know the rules of the road. No offense, but because you had to ask on a case like this, it’s better to spend ALOT more time on **studying (Istvan Urban’s book is well written for GBR), training (hands on), videos (you Tube or Dental Xp better yet) and then ask if you can watch a periodontist or OMFS that you refer to, do the case. This is much more in your interest then to keep experimenting. When you have a problem you, your team and patients lose confidence,…it’s a momentum killer. You You also have peri-apical radiolucencies on the molar…recent endo?? or refer to an endodontist.
I am not sure why all of the discussion about grafting as the only issue is the actual placement right up against the molar. Considering that an extraction socket or sockets are the same as a a 3 walled defect, even in the complete absence of a buccal plate, I have never seen an instance in which advanced GBR techniques are required. I would just remove the fixture and let the area heal organically but if you feel the need than any allograft material will suffice and you need not worry about any advanced techniques like others have suggested. This is a difficult concept for us dentist to comprehend but extraction sockets heal and have been healing for many years without our help and IMHO most of the grafts we do are more like osseoinhibitors and thankfully for us these sites heal in spite of our attempts to fool nature.
There are several issues in this case. First of all there appears to be apical radiolucencies around the first molar. Secondly, there may be communication between the implant and the sinus. And lastly, obviously there are bony defects around the implant. I think you need to remove the implant, graft it and wait 4-6 months before attempting another implant. At the same time I think you need to re-evaluate the molar