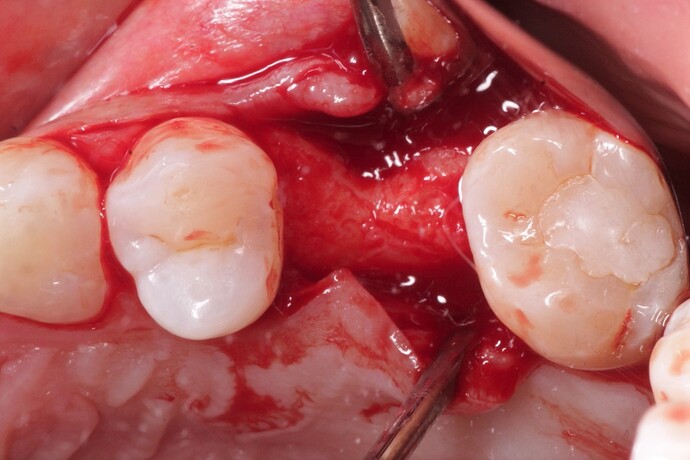
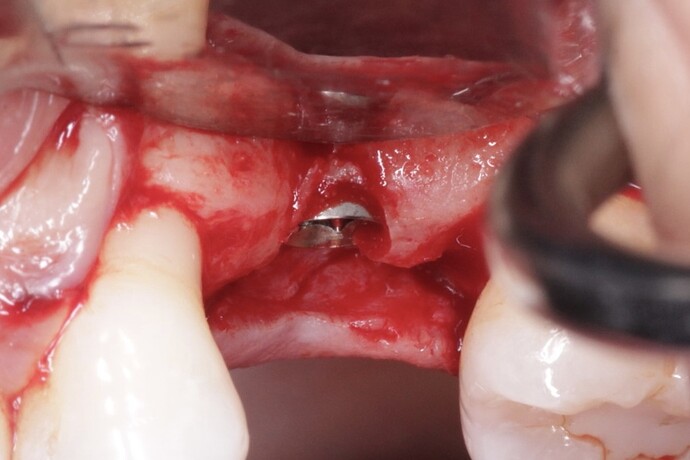
Considering the presentation of the ridge in this case, how would you approach augmentation of the buccal contour? Would you go for a GBR with bone + membrane OR just place a soft tissue substitute? What has your experience been with either of these?
This is a situation I would probably expand with Densah burs. possibly do a veneer graft on the buccal depending on the patient med/social/compliance history.
GBR + membrane
Will use autogenous first layer
The implant is stable and completely housed in bone thus it only requires a soft tissue augmentation. This is a textbook example of when to do a soft tissue ridge augmentation and any addition of bone dust +membrane while not contraindicated is completely unnecessary. The use of such is most likely the result of the individual clinicians inability to perform the soft tissue graft as the corporate sponsored implant related CE courses only focus on selling widgets. Just my opinion base on 15 years of teaching fully credentialed dentists attending a residency program.
Particulate cort/canc mineralized allograft under a thick slowly resorbing membrane such as Ossix Volumax.
I would have placed the implant a bit more palatal and that’s all. Less you play ,better is !
This soft tissue graft can easily be performed without creating an additional surgery as it can be rolled from the palatal side. This is an easy, though rarely taught in CE courses where selling products is the ultimate goal, procedure that I routinely do at no additional charge to the patient. I get a lot of patients coming for second opinion and the most common reason they choose me over the others is because I rarely see the need for graft+membrane+PRF +unicorn droppings etc… and by promoting healthy soft tissue these things just work great.
Can you please state your valid, worthwhile, and very helpful opinion without disparaging others? Is every CE course that teaches grafting/membrane out to just sell products? This is an absurd accusation, which simply diminishes the credibility of your extremely valuable insights. There is room for disagreement on every case without claiming the other side is just a bunch of idiots who know nothing. Incidentally, I do believe your take on this case, that a soft tissue graft is sufficient. I think we have another case coming soon that shows this. Thank you.
I whole heartedly believe that every corporate sponsored Implant CE course is designed to sell products and it definitely shows in the way the dental profession treatment plans. We have people believing that a graft and membrane are needed for every extraction in which an implant is placed… they certainly didn’t learn this from any valid text. I do not believe that the other side is idiots or wrong in any way as I too once felt that way until I separated myself from the indoctrination of corporate CE. Read the “scientific studies” as they call them and you will see manipulation of the data to illustrate a preconceived conclusion designed to promote a concept. It is fine to add every material under the sun to every implant site it is just not necessary… I am pretty sure that is fact and not opinion.
The concept that you never need to use a graft or another product is just as dubious as the concept that you always need to graft every case. Each case is different and should be planned based on its needs. Also, not all CE courses are sponsored by corporate entities. Its easy to tell the difference. I agree though, we need to be wary of much that we read or see in any course, even if not commercially sponsored.
In the above case, buccal bone is missing in the top one mm and appears thin in the next 2 or 3 mm. Sure, this implant would survive even if nothing additional is done, but in most patients, there would likely be a couple of mm gingival recession within a year or two exposing metal. The esthetic consequences may be important to many patients. In other patients there could be even greater loss of buccal bone resulting is an inflamed pocket, and dark shadowing through the overlying gingiva. Implant failure in these cases after a few years is not uncommon. It is so easy to augment the buccal bone to prevent these issues when it seems beneficial, such as in this instance.
Every course that teaches implants must have implants at the course and other materials. As such, every single implant course is by definition sponsored in some fashion, even if the company only donated all the products. Of course this has marketing benefits for the company that provides materials, but that doesn’t mean every single course is just some sales pitch or that there is hidden agenda. It depends. Many courses provide excellent educational opportunities with top clinicians, others not so much. Everyone has to use their own judgement on this.
As for grafting + membrane, I think you are just moving to an opposite extreme from your original indoctrination. The answer is probably in the middle, and really case dependent.
As for “scientific studies”, you are correct that in dental there really aren’t any double-blinded, randomized trials like you find in pharma, so it is difficult to really draw any definitive conclusions from much dental research. However, again this is not because of some hidden agenda, it’s just not feasible to do randomized trials in dentistry for many reasons. However, I think many studies are still perfectly legitimate and if you look at the totality of studies in a certain area of dental, and use some practical experience, it is clear what really works and is based on solid science.
Great comments with the expression of some passionate feelings. I am not put off by this, so long as the welfare of the patient is the focus of our efforts. I thinkthere should never be a surprise when the incision is made and the bone exposed. A CBCT image of this case would have been extremely helpful. I believe current guidelines call for at least 2 mm of buccal bone and 2 mm of attached gingival for a successful implant. If the CBCT shows this is deficient then consider repositioning the implant to the palatal. If repositioning to the palatal does not provide sufficient bone then a graft is necessary. Now we can discuss what graft material and technique.
The political debate this case stimulates shows how Dentistry is an industry in itself.
Bias is everywhere and mostly it is fine as it fuels the paper, event, course etc. sometimes it can get out of hand and can become the ‘assumed wisdom’
My issue with the current CE courses is that their solution for every deformity is osseous graft and membrane and it clearly shows in the way the profession treatment plans. I am not anti graft or membrane as I have a closet full of every combination you can imagine. Fact: I have been teaching dentists in a residency program for 15 years now and every one of them is familiar with basic implant placement and osseous grafting techniques though I have yet to encounter a single corporate CE trained clinician that can perform an autogenous soft tissue graft. When I was in training I had to demonstrate proficiency in soft tissue grafting before I was permitted to place implants because it is a critical piece of the puzzle. If I were treating this case I would first place a xenograft and cover it with an autogenous connective tissue graft. My only purpose for the xenograft it that it make me feel better to add some extra bulk under the connective tissue for more contour and I do not charge extra for this. I see treatment plans every day from various clinicians and they all include additional charges for grafts and membranes that can only be inspired by CE designed to improve the bottom line. If you don’t believe that bone grafts can succeed without a membrane I would suggest looking at some of the literature from the Wilko’s… no you will not find implants involved but you will see evidence of radiographic bone graft success in the absence of a collagen membrane. If the goal is to augment a truly deficient ridge so that it can accept an implant than GBR with graft and membrane of choice is certainly the gold standard but when contour is the goal then the patient should be spared the docs additional production$$. If you are so inclined as to use everything every time that is fine though only necessary in the eyes of the manufacturer promoting the course.
Agree except that I am still scratching my head as to where this magical number of 2mm buccal bone comes from. I used to do a lot of 2 stage implants where I would submerge them at placement and then expose them 3-6 months later. When doing this I was always amazed at how many solid/integrated/stable etc… fixtures would have exposed threads along the buccal but as long as the soft tissue was thick and healthy this never seems to matter. Again I think this magic 2mm number came from a sponsored CE designed to sell products and ignore soft tissue. Obviously having such a buccal plate is desirable but the necessity is questionable in the presence of healthy soft tissue.
There are plenty of publications that indicate the 2mm bone thickness guideline. Having placed thousands of implants for 38 years, 3 years of graduate implant training, a master’s degree in bone regeneration and being board certified in implant dentistry, I can confidently agree that this will recede. Too little blood flow on the dense cortical buccal bone for stability…no PDL blood flow. Perhaps the original GBR/Buser book should be part of the reading for your students training? Yes, I have alot of stuff too that I bought yet it turned out that I was simply excited about doing things better. All of us can talk about what we think we know, yet the research on this one is clear.