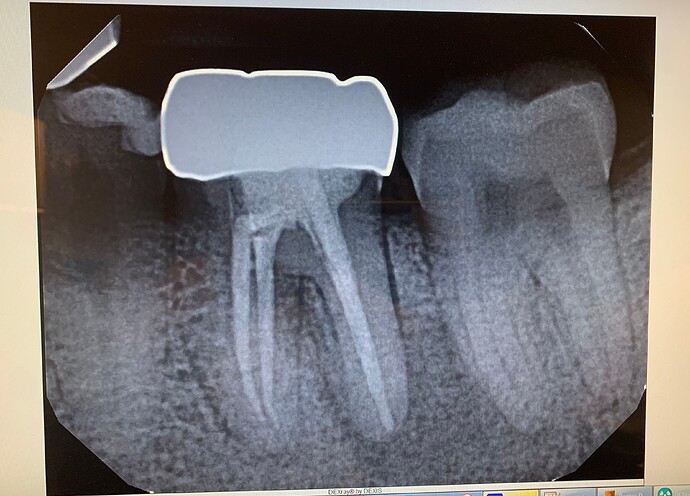
#19 chronic infection with fistula on the buccal. Would you do an immediate placement? What is your cut off for immediates if chronic infection present?
Thank you.
Oms comments:
I would not even consider immediate placement on a molar especially on an infected site. What’s the rush!Tim comments:
I have no problem placing an immediate implant in an infected site and it goes back to an article published by P.D. Miller regarding treating "hot lesions". In the presence of an infection there is an enormous amount of cellular activity and thus blood supply ready to be unleashed upon the removal of the (tooth) cause. In the article they were doing GTR procedures but I have found it to be true with implants as well. Think about extracting the infected tooth and just how rapidly it begins to heal. There is a considerable amount of subjective judgement but I tend to see active infection with an obvious underlying (tooth) cause to be a tremendous opportunity to get regeneration/bone growth and thus a great opportunity for a successful implant site. This is just my opinion and I do not always jump at the opportunity to place implants in infected site but under the right circumstances I would not consider an infected tooth to be a contraindication for immediate implant placement. One thing to keep in mind though when doing immediate molar implants is the height of the mesial and distal bone as it is really easy to place them too deep.... a friend of mine told me about this!!!OMS, PhD comments:
That article joins a plethora of anecdotal articles that make poor references to other studies to support a preconceived idea and are basically observational and "how I do things". The lack of peer reviewed, properly constructed and evidence based studies in our discipline is quite alarming. This assumption that infected sites are possibly good environments for healing is misguided.Basic microbiology and immunology has elucidated that bacterial lipopolysaccharide (more so in gram negative bacteria) is the main cause of periapical periodontitis because it stimulates the body’s local immune response. A large number of inflammatory cells are activated after the release of inflammatory mediators, cytokines and enzymes, leading to the destruction of the apical tissue, the formation of inflammatory granulation tissue, and alveolar bone destruction. (1)
LPS induces osteoclast formation through the RANKL pathway to support osteoclast survival and fusion. LPS also stimulates the secretion of tumor necrosis factor α (TNF-α) and induces cell transformation into osteoclasts.(4,5). Several studies have shown that LPS also directly induces osteoblast necrosis and apoptosis. In a study of fracture healing in an animal model, the injection of LPS delayed the healing of fractures and reduced the strength of the new bone. (6,7)
LPS induces osteoclast formation through the RANKL pathway to support osteoclast survival and fusion. LPS also stimulates the secretion of tumor necrosis factor α (TNF-α) and induces cell transformation into osteoclasts (11). LPS directly promotes the differentiation and proliferation of osteoclasts but inhibits the differentiation and proliferation of osteoblasts (12).
Thus, the dynamic balance between osteoblasts and osteoclasts is the critical link in the process of periapical bone remodeling as well as ultimately determining if the environment would be supportive of integrating well with hardware. (2). As such, there is suppression and up-regulation of osteoblasts and osteoclasts in periapical disease. For a long time it was not understood what regulates this relationship.
Many immunologic proteins are active in an apical infection. One of the main pathways in the cellular defense to pathogenic bacteria (and other pathogens) is the One such pathway that activates macrophages is the nuclear factor kappa B pathway (NF-kB). This pathway is commonly referred to as the Cellular Survival Pathway (3). Within this pathway, there are many immunologic modulators and one such glycoprotein is Osteopontin or OPN. OPN is a secreted phosphorylated glycoprotein that was first discovered in bone tissue.(8). It is a multifunctional matrix protein that is widely involved in the progression of bone-related diseases (9). A number of studies have shown that OPN promotes osteoclast adhesion and improves the osteocytes activity of osteoclasts. When the OPN gene was knocked out, the number of osteoclasts decreased significantly (9,10).
This is one of the many modulators and bioactive proteins that are involved in an infected that alters the normal response to injury like surgery that tip the scales from an osteoblast healthy environment to one of an osteoclast dominate environment. While bioactive proteins that stimulate angiogenesis may seems like a rich environment for healing, the pool of other negatively influencing cytokines, mediators, proteins, enzymes, etc. are present. From a biological, microbiological and immunological standpoint, the environment for implant placement in an infected site will never be a supportive as compared to a non-infected site. Also direct contamination of the implant by introduction to an infected site is another discussion all together.
Looking at the animal and the small sample sized human studies regarding implants in infected sites, the studies used relatively respectable statistical analysis but their criteria defining inclusions were heavily flawed. As such, they are using flawed data with good statistical analysis. What good is that? The majority of studies examined sites with chronic periapical infection; however, the classification of infection was often vague and not categorized to be related to the outcomes. However, in both models, when inclusion criteria are reasonable the difference is not as great as you would assume and it speaks to the dynamic and resilient immunological response of the host.
That being said, as an expert witness in cases like this, it is difficult to overcome both “standard of care” and “best practices”. If you have a catastrophic failure in a case where implants were introduced to an infected site(s), you may find yourself struggling to find qualified experts to present qualified research evidence to support your decision. The other side will find plenty of qualified experts not only being surgeons but also biologists, biochemists, immunologists, microbiologists, statisticians, histologists, and a whole bunch of others a prudent attorney will retain (provided the case has a potential dollar value to support such a bullpen of experts). Most court battles are won and lost by the experts. The biggest hurdle will play out if you have a jury trial versus a bench trial. It is almost impossible to overcome the idea to a layperson that any procedure has a higher risk of complications in an infected site versus a clean and healthy site despite what ever evidence is presented. That notion has been engrained in everyone’s head since they can remember (your “boo-boo” your mom cleaned with Bactine or mecurochrome or whatever and placed a band-aid over).
Commercials about antiseptics and antiseptic band-aids are fairly prevalent in society.
So you have to ask yourself is it worth it? Probably antibiotics and excellent local control and for the most part your cases go well. But what happens when they do not in these situations? Then what? Trying to defend your actions to an inquisitive patient using a less than optimal paper may not be the best tactic. What’s the harm in doing it the better way with a better environment for success? Even in an infected site if it is “successful” will you achieve the best quality adaptive bone to stress possible? There are lots of studies and current studies looking at just that.
- Kawashima N, Suzuki N, Yang G, Ohi C, Okuhara S, Nakano-Kawanishi H, Suda H: Kinetics of RANKL, RANK and OPG expressions in experimentally induced rat periapical lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103: 707-711
- Undale A, Srinivasan B, Drake M, McCready L, Atkinson E, Peterson J, Riggs BL, Amin S, Modder UI, Khosla S: Circulating osteogenic cells: Characterization and relationship to rates of bone loss in postmenopausal women. Bone2010; 47: 83-92
- Albensi Benedict C. What Is Nuclear Factor Kappa B (NF-κB) Doing in and to the Mitochondrion? Frontiers in Cell and Developmental Biology. 2019. Volume 7, Page 254.
- Kaomongkolgit R, Manokawinchoke J, Sanchavanakit N, Pavasant P, Sumrejkanchanakij P: Fibronectin supports TNF-alpha-induced osteopontin expression through beta1 integrin and ERK in HN-22 cells. Arch Oral Biol 2010; 55: 101-107
- Joung YH, Darvin P, Kang DY, Sp N, Byun HJ, Lee CH, Lee HK, Yang YM: Methylsulfonylmethane inhibits RANKL-Induced osteoclastogenesis in BMMs by suppressing NF-kappaB and STAT3 activities. Plos One 2016; 11:e159891
- Rittling SR, Craig Z, Kader Y, Stephen S, Noriyuki S: Protective role of osteopontin in endodontic infection. Immunology 2010; 1: 105-114
- Singh R, Hui T, Matsui A, Allahem Z, Johnston CD, Ruiz-Torruella M, Rittling SR: Modulation of infection-mediated migration of neutrophils and CXCR2 trafficking by osteopontin. Immunology 2017; 150: 74-86.
- Chen J, Singh K, Mukherjee BB, Sodek J: Developmental expression of osteopontin (OPN) mRNA in rat tissues: Evidence for a role for OPN in bone formation and resorption. Matrix 1993; 13: 113-123.
- Tao X, Juxiang C, Yicheng L, Jinxu Z: Lentiviral-mediated siRNA against osteopotin in U251 glioma cell line. J Med Colleges PLA 2010: 1-10.
- Xu ST, Zou FZ, Cai LN, Xu WL: The downregulation of OPN inhibits proliferation and migration and regulate activation of Erk1/2 in ECA-109 cells. Int J Clin Exp Med 2015; 4: 5361-5369
- Joung YH, Darvin P, Kang DY, Sp N, Byun HJ, Lee CH, Lee HK, Yang YM: Methylsulfonylmethane inhibits RANKL-Induced osteoclastogenesis in BMMs by suppressing NF-kappaB and STAT3 activities. Plos One 2016; 11:e159891.
- Dong M, Yu X, Chen W, Guo Z, Sui L, Xu Y, Shang Y, Niu W, Kong Y: Osteopontin Promotes Bone Destruction in Periapical Periodontitis by Activating the NF-κB Pathway. Cell Physiol Biochem 2018;49:884-898.
Tim comments:
This is an impressive lit review and scientific justification as I am sure Dr. Anthony Fauci can produce plenty of evidence to support his crippling recommendations. While I depend on scientific justification in my every day practice I can’t help but acknowledge that some things occur naturally in nature despite scientific evidence to the contrary… like the rapid bone healing following the extraction of an infected tooth.Eric R comments:
I'm an OS, and I would not do an immediate here, and prefer never, although I do a few as long as the patient knows the success rate goes down from my 99.6 rate for graft-wait 3 months-implant-wait 3 months-uncover. Even with immediate, one needs to wait without a tooth for a few months. Why compromise?Anonymous Anonymous comments:
Would need to see the 3d imaging to see location of IAN and buccal and lingual bone. Even with that given the amount of infection I would extract, debride socket and graft.Russell Ollerton comments:
I have 30 years experience in placing and restoring implants. It all depends on the degree of the infections. I've had success and failures which has made me more conservative over time. As opposed to "increased blood supply" there can also be compromised healing due to the degree and chronic nature of the infection. If in doubt, extract and graft. At times you will find that the graft results are lacking and it is then that you should be grateful that you did not do an immediate placement into a compromised site.Greg Kammeyer, DDS, MS comments:
I've been placing immediate implants in molar sites for 10 -11 years. I'm delighted with how few problems there are, even with infection. Certainly there are a very few i choose not to implant immediately, like those that have a significant loss of buccal plate. I would use a cross linked membrane under the buccal periosteum if it has drainage there or on the lingual. I do routinely curette and run a round burr around the socket to decrease the bacterial count. With L-PRF in the bone graft, the white blood cells and growth factors stimulate Veg-F, and hence angiogenesis. I over pack the bone graft in height as some bone will be lost on socket grafts. The challenge on the mandible is fixation above the IAN. I am not fond of wide body implants for immediate molars as they put pressure on the thin buccal plate. In the maxilla, the floor of the sinus is great for primary stability. The literature supports predictably implanting in infected sites. Check it out. It's not about being in a hurry, anymore than taking out 3rd's in 15 minutes is. It's about practice philosophy, knowledge and comfort with a procedure. Dr Paul Fugazzoto has DVD's on how he does this procedure. I note patients don't want multiple treatment visits, if avoidable....as long as I get predictability.Aquiles Mas comments:
Immediate is best if possible. Get them on string antibiotics early. Curette the hell out of the site and irrigate well. Graft well. And these other guys have filled in the rest for you. It is only when I cannot achieve primary stability that I don’t put a fixture in. Otherwise fill in the hole and let the body do the work for you.Anonymous Anonymous comments:
Thank you everybody! The specialists are divided. I will extract, degranulate graft and wait 3 mo before the placement.Tim comments:
As one (periodontist)who has no issue placing an immediate implant into an infected site I think it is quit reasonable and safe to do in stages. My question is if an implant can’t be placed into this infected site then why should we feel comfortable introducing a bone graft material into the site. Are they not both essentially sterile foreign materials?guest comments:
If you look at it from a prosthetic perspective allowing the site to be grafted and healed is preferable to doing an immediate. Love looking at the “tomato on a stick” crowns on implants placed in immediate sites😳CONAN TENG DDS comments:
For posterior teeth. this is always the debate. Immediate or delayed implant placement. In this case, sufficient interceptal bone but possible buccal dehiscence or fenestration resulting in buccal sinus tract (not fistula). All too common for RCT molars. Safest and most predictable would be DELAYED IMPLANT PLACEMENT which this dr finally decide to do. 2 disadvantages are prolonged treatment, blunted papilla (which most dont care in the posterior) and twice the surgery. But waiting for bone turnover will result in an easier implant placement on a leveled alveolar ridge. Immediate implant placement pose challenges in placing implant in the interceptal bone or mesial/distal alveolar root socket. And the buccal defect means grafting and either place or not place a collagen membrane to cover the buccal defect. plus due to unpredictable healing/bone resorption. Do you place the implant Equi-osseous or sub-osseous? also because even with underprepare osteotomy the immediate implant may not have +35Ncm torque or good ISQ. So the implant can either be a spinner or need to be buried. This poses more challenges. However immediate implant placement eliminates one surgery and also shortens treatment time by 4 months. There is no right answer here. Different strokes for different folks. All depends the dr's comfort level in immediate or delayed implant placement. or pt financial circumstances (maybe pt cannot afford an implant now but can 5 months later), post extraction alveolar socket. Pts anatomy, etc. We as drs have to balance and judge. Sometimes have to wait. sometimes we can place implant right away. it's not on a whim, but educated and calculated plan. good luck dr. in a couple months should be implant placement. any updates? i would like to know please.